Drop Date: November 2011
SBB – Inflammation, Psychosocial Stress, and Salivary Cytokines
In This Drop: Salivary Bioscience, Inflammation and its Effects on Human Health

The study of inflammation and its effects on human health has been a major topic of interest in recent decades. Numerous studies have observed that a low-level state of systemic inflammation is a common feature found in metabolic diseases such as obesity, insulin resistance, and diabetes, as well as in a range of other conditions including cardiovascular disease, cancer, and autoimmune diseases. (See review by Hotamisligil 2006) This common inflammatory state involves a shift in the balance of pro- and anti-inflammatory polypeptide mediators known as cytokines, which in turn leads to changes in levels other inflammatory biomarkers, including acute phase proteins such as C-reactive protein. (Ganter, et al. 1989)
In addition to these changes in physical health, studies have also found that systemic inflammation can be involved in changes in brain health. Psychoneuroimmunologists now recognize that the brain and the immune system communicate through a group of common signaling molecules, which include cytokines, neuropeptides, and neurotransmitters. (See retrospective reviews: Blalock 2005, Dantzer & Kelley 2007, Dinarello 2007, and Irwin 2008.) The details of how peripheral cytokines communicate with the brain are not yet entirely clear, but a number of likely pathways have been proposed and are under investigation. Once these cytokine signals reach the brain they are believed to influence the levels of mood-relevant neurotransmitters such as serotonin, norepinephrine, and dopamine, which then affect behavior.
One major development in this field has been the realization that the connection between the brain and peripheral inflammation works in a bi-directional fashion. Studies have shown that psychosocial stress can activate the systemic inflammatory cytokine response, and it is believed that this response in turn can lead back to changes in brain function and the development of mental diseases such as major depressive disorder. (See reviews: Debnath, et al. 2011; Leonard 2010; Miller, et al. 2009; and Dantzer, et al. 2008)
Questions concerning the relationship between inflammation and the brain remain to be resolved, however. For example, it is uncertain whether systemic inflammation alone accelerates the progression of psychiatric disorders, or whether the peripheral and central inflammatory systems operate in parallel to increase the risk of the disorders. (Debnath, et al. 2011) Additionally, it has been noted that inflammatory markers are not always elevated in clinically depressed patients. (Dantzer, et al. 2008)
The review by Miller et al. summarizes a pathway by which stress, operating through the sympathetic nervous system (SNS), can lead to elevated peripheral cytokine levels. In this scheme, catecholamines released from the SNS act through alpha- and beta-adrenergic receptors on macrophages and other immune cells to activate signaling pathways, including the inflammatory transcriptional factor NF-κB. NF-κB signaling then induces the immune cells to release pro-inflammatory cytokines in response to the stress.
Since uncontrolled inflammation has negative effects on health, the brain recognizes the elevated systemic cytokine levels and induces the HPA axis to increase cortisol secretion, which dampens the inflammatory response by inhibiting the NF-κB signaling. Inhibitory parasympathetic nervous system (PNS) activity and possibly feedback mechanisms within the SNS are also thought to be involved in the control of the inflammatory response. (Rohleder 2011; Sternberg 2006)
Salivary Cytokines
Research involving salivary cytokines has grown over the last decade, and these studies have most often focused on periodontal disease or other oral diseases such as Sjögren’s syndrome, oral lichen planus, and fungal infections. The study of the inflammatory cytokine response to stress has largely utilized in vitro or serum measurements of these markers, but studies are now beginning to explore relationships between stress, brain function, and salivary cytokines, as well.
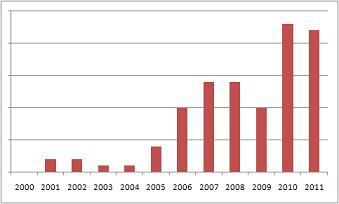
Figure 2. Growth in studies discussing salivary IL-6, 2000-2011.
A major issue that has prevented salivary cytokines from becoming more widely adopted in general psychobiological research is that studies have generally found that salivary levels of these markers correlate only modestly to serum values. (Minetto, et al. 2005; Sjögren, et al. 2006; Fernandez-Botran, et al. 2011) The apparent lack of correlation is not surprising, due to the multiple paths of entry into saliva that exist for these biomarkers. In addition to being produced locally in the saliva glands, cytokines are produced in a variety of mucosal tissues and immune cells in the mouth, and they may also enter through micro-injuries or by transudation from blood. (Schapher, et al. 2011; Dongari-Bagtzoglou, et al. 2005) The permeability of membranes in oral tissues changes in response to infection and inflammation, hormone levels, and – as is suggested in one of the studies featured in this issue – perhaps even by autonomic nervous control; both long- and short-term changes in the contributions from blood are therefore likely to occur.
Because the salivary glands and other tissues in the mouth are also affected by the same outflow of autonomic nervous signals that govern systemic cytokine increases, it seems likely that salivary cytokines will be found to have uses in psychobiological studies. The next generation of studies will need to explore these markers carefully in order to understand the nature of their relationships to stress and various disease states.
To illustrate the potential value of salivary cytokines for biomedical research, in this issue of The Spit Report we feature several research papers that have examined relationships between psychosocial stress, salivary cytokines, and brain function related to mental health. In addition, a small number of exploratory studies have also begun to appear in recent years that have reported relationships between salivary cytokines and diseases in tissues remote from the oral cavity; examples of these are included below under Additional Reading.
Technical Advice
Collecting and Handling Saliva Samples for Cytokine Analysis
Studies that include measurements of cytokines in saliva are increasing in number, but information on the best ways to collect and handle the saliva samples is still limited for these analytes.
*Salimetrics provides this information for research use only (RUO). Information is not provided to promote off-label use of medical devices. Consult full text of article.
Featured Articles
Relations Between Mucosal Immunity and Children’s Mental Health: The Role of Child Sex.
Keller, P.S., El-Sheikh, M., Vaugh, B., & Granger, D.A. (2010).Brain Physiol Behav, 101(5), 705-12.
Secretory IgA (SIgA) and interleukin-6 (IL-6) were measured in saliva samples taken from children in order to examine relations between salivary immune parameters and children’s mental health. Higher levels of SIgA were found to be associated with greater impulsivity, delinquency, and emotional distress in girls. Higher levels of salivary IL-6 were found to be associated with self-reported depression and anxiety, as well as parent-reported impulsivity and social withdrawal, emotional distress, and delinquency in girls. Higher SIgA was marginally associated with lower impulsivity and emotional distress in boys. Results for salivary IL-6 and mental health were consistent with findings from studies involving serum IL-6, while the findings for SIgA showed different results than those of several studies with adults.
Research Area: Stress, Behavior & Development; Health & Inflammation
Focus: Behavioral Disorders; Social Behavior & Emotions; Inflammation & Immune Function
When Grief Heats Up: Proinflammatory Cytokines Predict Regional Brain Activation.
O’Connor M.-F., Irwin, M.R., & Wellisch, D.K. (2009). Neuroimage, 47(3), 891-96.
Salivary levels of two pro-inflammatory cytokines, interleukin-1β (IL-1β) and soluble tumor necrosis factor receptor II (sTNFrII) were measured in women in bereavement who underwent fMRI scans during a grief-elicitation task. Analyses revealed that salivary levels of both markers were positively associated with regional brain activation and emotional processing. The results support the idea that peripheral inflammation (in the mouth) is communicated to the brain, and that the resulting changes in motivational state may influence emotional processing.
Research Area: Stress, Behavior & Development; Health & Inflammation
Focus: Social Behavior & Emotions; Inflammation & Immune Function
The Effect of Disgust on Oral Immune Function.
Stevenson, R.J., Hodgson, D., Oaten, M.F., Barouei, J. & Case, T.I. (2011). Psychophysiology, 48(7), 900-907.
An experimental group of participants viewed images that were intended to induce disgust, as compared to negative and neutral induction control groups. Saliva was collected at three time points in order to monitor changes in levels of secretory IgA (SIgA) and tumor necrosis factor-alpha (TNF-α), as indicators of immune function and oral inflammation, respectively. Participants in the disgust group showed decreases in SIgA and increases in TNF-α, compared to the negative and neutral control groups. Increases in TNF-α were accompanied by increases in salivary albumin, an indication of increased membrane permeability to serum components. The authors suggest that the increases in TNF-α and the accompanying rise in albumin are in response to increased autonomic nervous activity related to the disgust condition.
Research Areas: Stress, Behavior & Development; Health & Inflammation
Focus: Autonomic Nervous System; Inflammation & Immune Function
Interleukin-6 Levels in Relation to Psychosocial Factors: Studies on Serum, Saliva, and In Vitro Production by Blood Mononuclear Cells.
Sjögren, E., Leanderson, P., Kristenson, M., & Ernerudh, J. (2006). Brain Behav Immun, 20(3), 270-78.
IL-6 levels were analyzed in serum, saliva, and in the supernatants of cell cultures stimulated in vitro with lipopolysaccharide. IL-6 levels in serum and saliva were found to be negatively related to psychosocial resources and positively related to psychosocial risk factors, with the opposite findings for LPS stimulated supernatants. No correlation was found between IL-6 levels in serum and saliva. The results support the view that IL-6 is involved in mediating the risk for disease development that has been associated with psychosocial factors.
Research Areas: Stress, Behavior & Development; Health & Inflammation
Focus: Social Behavior & Emotions; Inflammation & Immune Function
REFERENCES & RELATED RESEARCH
- Aurer, A., Aurer‐Koželj, J., Stavljenić‐Rukavina, A., Kalenić, S., Ivić‐Kardum, M., & Haban, V. (1999). Inflammatory mediators in saliva of patients with rapidly progressive periodontitis during war stress induced incidence increase. Coll Antropol, 23(1), 117‐24.
- Boumba, D., Skopouli, F.N., & Moutsopoulos, H.M. (1995). Cytokine mRNA expression in the labial salivary gland tissues from patients with primary Sjögren’s syndrome. Br J Rheumatol, 34(4), 326‐33.
- Brennan, M.T., & Fox, P.C. (2000). Cytokine mRNA expression in the labial salivary glands of healthy volunteers. Oral Dis, 6(4), 222‐26.
- Catov, J.M., Bodnar, L.M., Ness, R.B., Barron, S.J., & Roberts, J.M. (2007). Inflammation and dyslipidemia related to risk of spontaneous preterm birth. Am J Epidemiol, 166(11), 1312‐19.
- Chiappelli, F., Iribarren, F.J., & Prolo, P. (2006). Salivary biomarkers in psychobiological medicine.
- Bioinformation, 1(8), 331‐34.
- Chrousos, G.P. (2009). Stress and disorders of the stress system. Nat Rev Endocrinol, 5(7), 374‐81.
- Cox, A.J., Pyne, D.B., Gleson, M., & Callister, R. (2008). Resting plasma and salivary IL‐6 concentrations are not correlated in distance runners. Eur J Appl Physiol, 103(4), 477‐79.
- Dickerson, S.S., Kemeny, M.E., Aziz, N., Kim, K.H., & Fahey, J.L. (2004). Immunological effects of induced shame and guilt. Psychosom Med, 66(1), 124‐31.
- Dugué, B., Ilardo, C., Aimone‐Gastine, I., Guéant, J.L., Mouzé‐Amady, M., Cnockaert, J.C., Mur, J.M., et al. (1996). Cytokines in saliva: Basal concentrations and the effect of high ambient heat (sauna). Stress Med, 12(3), 193‐97.
- El‐Sheikh, M., Buckhalt, J.A., Granger, D.A., Erath, S.A., & Acebo, C. (2007). The association between children’s sleep disruption and salivary IL‐6. J Sleep Res, 16(2), 188‐97.
- Fernández‐Sánchez, A., Madrigal‐Santillán, E., Bautista, M., Esquivel‐Soto, J., Morlaes‐González, Á., Esquivel‐Chirino, C., Durante‐Montiel, I., Sánchez‐Rivera, G., Valadez‐Vega, C., & Morales‐González, J.A. (2011). Inflammation, Oxidative Stress, and Obesity. Int J Mol Sci, 12(5), 3117‐32.
- Fox, P.C., Brennan, M., & Di Sun, P. (1999). Cytokine expression in human labial minor salivary gland epithelial cells in health and disease. Arch Oral Biol, 44(Suppl 1), S49‐S52.
- Fox, R.I., Kang, H.I., Ando, D., Abrams, J., & Pisa, E. (1994). Cytokine mRNA expression in salivary gland biopsies of Sjogren’s syndrome. J Immunol, 152(11), 5532‐39.
- Giannobile, W.V., Beikler, T., Kinney, J.S., Ramseier, C.A., Morelli, T., & Wong, D.T. (2009). Saliva as a diagnostic tool for periodontal disease: Current state and future directions. Periodontology 2000, 50, 52‐64.
- Gill, J., Vythilingam, M., & Page, G.G. (2008). Low cortisol, high DHEA, and high levels of stimulated TNFα, and IL‐6 in women with PTSD. J Trauma Stress, 21(6), 530‐39.
- Gold, S.M., & Irwin, M.R. (2009). Depression and immunity: Inflammation and depressive symptoms in multiple sclerosis. Immunol Allergy Clin North Am, 29(2), 309‐20.
- Groer, M., Murphy, R., Bunnell, W., Salomon, K., Van, Eepoel, J., Rankin, B., et al. (2010). Salivary measures of stress and immunity in police officers engaged in simulated critical incident scenarios. J Occup Environ Med, 52(6), 595‐602.
- Holmes, C., Cunningham, C., Zotova, E., Woolford, J., Dean, C., Kerr, S., Culliford, D., & Perry, V.H. (2009). Systemic inflammation and disease progression in Alzheimer disease. Neurology, 73(10), 768‐74.
- Liezmann, C., Klapp, B., & Peters, E.M.J. (2011). Stress, atopy and allergy: A re‐evaluation from a psychoneuroimmunologic perspective. Dermatoendocrinol, 3(1), 37‐40.
- Llamas Moya, S., Boyle, L., Lynch, P.B., & Arkins, S. (2006). Pro‐inflammatory cytokine and acute phase protein responses to low‐dose lipopolysaccharide (LPS) challenge in pigs. Animal Sci, 82, 527‐34.
- Lumeng, C.N. & Saltiel, A.R. (2011). Inflammatory links between obesity and metabolic disease. J Clin Invest, 121(6), 2111‐17.
- Mastrolonardo, M., Alicino, D., Zefferino, R., Pasquinie, P., & Picardi, A. (2007). Effect of psychological stress on salivary interleukin‐1β in psoriasis. Arch Med Res, 38(2), 206‐11.
- Miller, C.S., Foley, J.D., Bailey, A.L., Campell, C.L., Humphries, R.L., Christodoulides, N., Floriano, P.N., et al. (2010). Current developments in salivary diagnostics. Biomark Med, 4(1), 171‐89.
- Minetto, M.A., Gazzoni, M., Lanfranco, F., Baldi, M., Saba, L., Pedrola, R., Komi, P.V., et al. (2007). Influence of the sample collection method on salivary interleukin‐6 levels in resting and post‐exercise conditions. Eur J Appl Physiol, 101(2), 249‐56.
- Moons, W.G., Eisenberger, N.I., & Taylor, S.E. (2009). Anger and fear responses to stress have different biological profiles. Brain Behav Immun, 24(2), 215‐19.
- Moutsopoulos, N.M. & Madianos, P.N. (2006). Low‐grade inflammation in chronic infectious diseases: Paradigm of periodontal infections. Ann N Y Acad Sci, 1088, 251‐64.
- Nielsen, A.A., Nielsen, J.N., Schmedes, A., Brandslund, I., & Hey, H. (2005). Saliva Interleukin‐6 in patients with inflammatory bowel disease. Scand J Gastroenterol, 40(12), 1444‐48.
- Nishanian, P., Aziz, N., Chung, J., Detels, R., & Fahey, J.L. (1998). Oral fluids as an alternative to serum for measurement of markers of immune activation. Clin Diag Lab Immunol, 5(4), 507‐12.
- O’Connor, M.‐F., Bower, J.E., Cho, H.J., Creswell, J.D., Dimitrov, S., Hamby, M.E., Hoyt, M.A., et al. (2009). To assess, to control, to exclude: Effects of biobehavioral factors on circulating inflammatory markers. Brain Behav Immun, 23(7), 887‐97.
- Palmqvist, P., Lundberg, P., Lundgren, I., Hänström, & Lerner, U.H. (2008). IL‐1β and TNF‐α regulate IL‐ 6‐type cytokines in gingival fibroblasts. J Dent Res, 87(6), 558‐63.
- Pekiner, F.N., Bumru, B., Demirel, G.Y., & Ozbayrak, S. (2009). Burning mouth syndrome and saliva: Detection of salivary trace elements and cytokines. J Oral Pathol Med, 38(3), 269‐75.
- Peruzzo, D.C., Benatti, B.B., Ambrosano, G.M., Nogueira‐Filho, G.R., Sallum, E.A., Casati, M.Z., & Nociti, F.H., Jr. (2008). A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J Periodontol, 78(8), 1491‐504.
- Pike, J.L., Smith, T.L., Hauger, R.L., Nicassio, P.M., Patterson, T.L., McClintick, J., Costlow, C., & Irwin,
- M.R. (1997). Chronic life stress alters sympathetic, neuroendocrine, and immune responsivity to an acute psychological stressor in humans. Psychosom Med, 59(4), 447‐57.
- Preliasco, V.F., Benchuya, C., Pavan, V., de la Cal, C., Ganzinelli, S., & Sterin‐Borda, L. (2008). IL‐1β and PGE2 levels are increased in the saliva of children with Langerhans cell histiocytosis. J Oral Pathol Med, 37(9), 522‐27.
- Rhodus, N.L., Cheng, B., Myers, S., Bowles, W., Ho, V., & Ondrey, F. (2005). A comparison of the pro‐ inflammatory, NF‐κB‐dependent cytokines: TNF‐alpha, IL‐1‐alpha, IL‐6, and IL‐8 in different oral fluids from oral lichen planus patients. Clin Immunol, 114(3), 278‐83.
- Ruhl, S., Hamberger, S., Betz, R., Sukkar, T., Schmalz, G., Seymour, R.A., Hiller, K.‐A., & Thomason, J.M. (2005). Salivary proteins and cytokines in drug‐induced gingival overgrowth. J Dent Res, 83(4), 322‐26.
- Sato, J., Goto, J., Murata, T., Kitamori, S., Yamazaki, Y. Satoh, A., & Kitagawa, Y. (2010). Changes in saliva interleukin‐6 levels in patients with oral squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 110(3), 330‐6.
- Skopec, R. (2011). Mechanism linking aggression stress through inflammation to cancer. J Cancer Sci Ther, 3(5), 134‐39.
- Souza, P.P., Palmqvist, P., Lundgren, I., Lie, A., Costa‐Neto, C.M., Lundberg, P., & Lerner U.H. (2010). Stimulation of IL‐6 cytokines in fibroblasts by toll‐like receptors 2. J Dent Res, 89(8), 802‐7.
- Tanda, N., Ohyama, H., Yamakawa, M., Ericsson, M., Tsuji, T., McBride, J., Elovic, A., Wong, D.T., & Login, G.R. (1998). IL‐1β and IL‐6 in mouse parotid acinar cells: Characterization of synthesis, storage, and release. Am J Physiol, 274(1 Pt 1), G147‐G156.
- Tobón‐Arroyave, S.I., Jaramillo‐González, P.E., Isaza‐Guzmán, D.M. (2008). Correlation between salivary IL‐1β levels and periodontal clinical status. Arch Oral Biol, 53(4), 346‐52.
- Weik, U., Herforth, A., Kolb‐Bachofen, V., & Deinzer, R. (2008). Acute stress induces proinflammatory signaling at chronic inflammation sites. Psychosomatic Med, 70(8), 906‐912.
- Wellen, K.E., & Hotamisligil, G.S. (2005). Inflammation, stress, and diabetes. J Clin Invest, 115(5), 1111‐
- 1119.
- Yao, C., Li, X., Murdiastuti, K., Kosugi‐Tanaka, C., Akamatsu, T., Kanamori, N., & Hosoi, K., (2005). Lipopolysacccharide‐induced elevation and secretion of interleukin‐1β in the submandibular gland of male mice. Immunology, 116(2), 213‐22.
- Youinou, P., Taher, T.E., Pers, J.O., Mageed, R.A., & Renaudineau, Y. (2009). B lymphocyte cytokines and rheumatic autoimmune disease. Arthrit Rheum, 60(7), 1873‐80.
- Zunt, L.L., Burton, L.V., Goldlatt, L.I., Dobbins, E.E., & Srinivasan, M. (2009). Soluble forms of Toll‐like receptor 4 are present in human saliva and modulate tumour necrosis factor‐α secretion by macrophage‐like cells. Clin Exp Immunol, 156(2), 285‐93.
*Note: Salimetrics provides this information for research use only (RUO). Information is not provided to promote off-label use of medical devices. Please consult the full-text article.
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)